The monkeypox virus has become a rising topic in media, just as the COVID-19 pandemic is starting to loosen its grip on society. The feeling is familiar to the early months of 2020 before COVID-19 surged the nation.
UNF Public Health Educator Dr. Amber Barnes explained the current state of the monkeypox virus, as well as its history and characteristics.
Is there a risk of another outbreak like COVID-19?
“The current monkeypox outbreak has not reached the threshold for a pandemic declaration as of today,” Dr. Barnes wrote in her statement.
However, she also says that if it does spread, it “would allow more funding and research opportunities to address the outbreak in real-time and should not indicate an increase in severity of the virus or instill panic.”
Rest assured, the risk of exposure to monkeypox is rare, and people typically recover from the infection. There have been 790 cases of the monkeypox virus and orthopox virus reported in 28 different countries, as of June 2, according to the CDC.
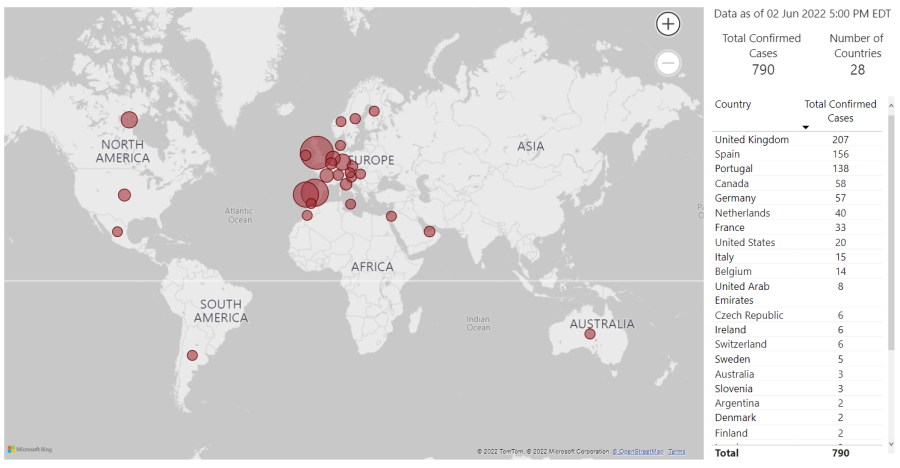
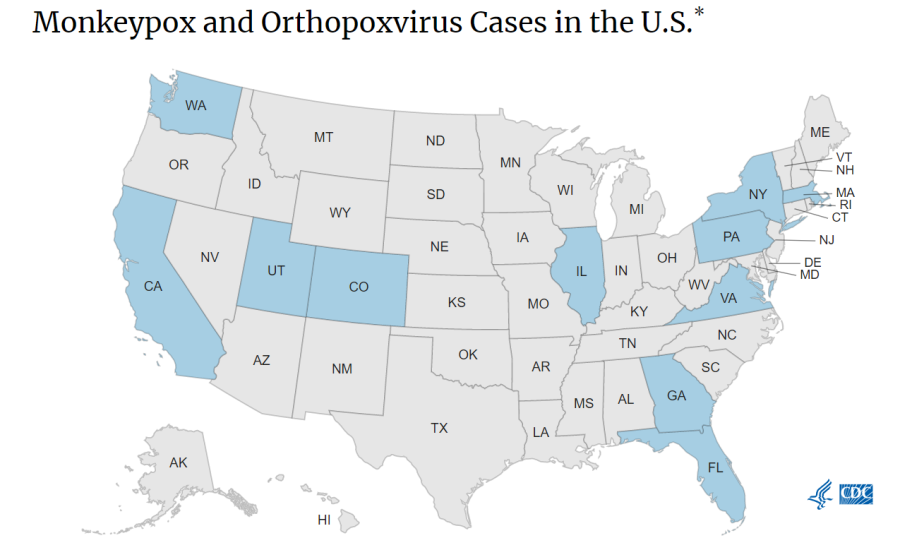
The United States has 21 reported cases in the states highlighted blue in the graphic. Florida currently has three reported cases as of June 2.
Fatal cases mostly occur among immunocompromised people in endemic countries. Since monkeypox is so similar to smallpox, those with the smallpox vaccine may have some “cross-reactive protection,” Dr. Barnes said.
“With Covid-19, the health care and epidemiological communities were trying to understand a brand new virus without a rulebook,” Dr. Barnes said. “Thankfully, with monkeypox, we are familiar with the virus, its symptoms, its transmission routes, testing procedures, and prevention strategies.”
What do we know about where Monkeypox came from and how it spreads?
“Monkeypox is not a new virus,” Dr. Barnes explained. It got its name in 1958 when it was discovered in laboratory monkeys in Denmark. She says that the first human case of this disease was identified in 1970 in a child from the Democratic Republic of the Congo, but it was likely circulating among people for much longer.
Dr. Barnes also explained that human cases are not uncommon in endemic areas, such as West and Central Africa, and that human cases in other parts of the world are likely a result of the importation of infected animals.
She gave examples of a 2003 outbreak in the United States associated with pet prairie dogs imported from Ghana where there were 71 cases. Another example from 2018 includes travel-acquired infections among travelers from the UK and Israel returning home from visiting Nigeria.
“While we are still not sure which animal species may be the natural reservoir or how it may be transmitted between animals, humans can be exposed to the monkeypox virus from contact with infected animals or animals products (e.g. bites or scratches from an infected animal, inadequately prepared/undercooked meat, etc.),” Dr. Barnes wrote.
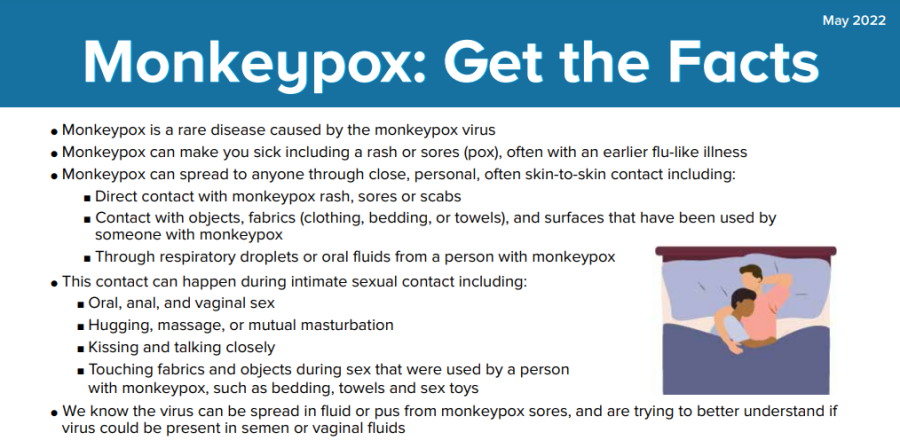
Humans are at risk of transmission through direct contact with an infected person or their personal items. This can happen through contact with:
- skin lesions or sores
- bodily fluids
- respiratory droplets
- inanimate objects that an infected person may be using such as bedding, towels, or articles of clothing.

Researchers aren’t yet sure if monkeypox can be transferred in semen or vaginal fluids, but they know that it can be transmitted from acts of intimacy such as sex, kissing, cuddling and more.
“The current outbreak of monkeypox is quite unique because there doesn’t seem to travel to endemic areas among positive or suspected cases,” Dr. Barnes explained. “Many infected individuals are being discovered by primary care physicians or from providers for sexual health services. As of May 13, 2022, cases have been found in 23 countries that we would not expect to have cases (non-endemic countries), including the United States.”
Dr. Barnes also mentioned that many of the cases in the current outbreak are men who have sex with men (MSM) and that it’s likely that monkeypox has been spreading through close contact between sex partners for a while before it was noticed and reported by physicians.
“This suggests that it may be possible to spread the virus before symptoms appear, but this has not been established, and researchers are currently investigating transmission risks and symptom onset associated with the current outbreak,” she explained.
What kind of treatment is available for Monkeypox patients?
“Most people who get monkeypox will recover on their own because monkeypox does not have the same potential for complications or fatality rate associated with something like Covid-19,” Dr. Barnes said. “Treatment is generally supportive.”
Health care providers would want to test anyone who has had contact with a confirmed or suspected case, has traveled to an endemic area of West or Central Africa (including other areas that are a current hotspot), or who has symptoms, according to Dr. Barnes. If the tests confirm the diagnosis, the patient will be asked to isolate, and they will be monitored.
Infection symptoms may begin with:
- Fever
- Headache
- Muscle aches
- Backache
- Swollen lymph nodes
- Chills
- Exhaustion
The person may then develop a:
- Rash (typically on the face and then moving to other parts of the body)
- Skin lesions that go from:
- Macules
- Papules
- Vesicles
- Pustules
- Scabs
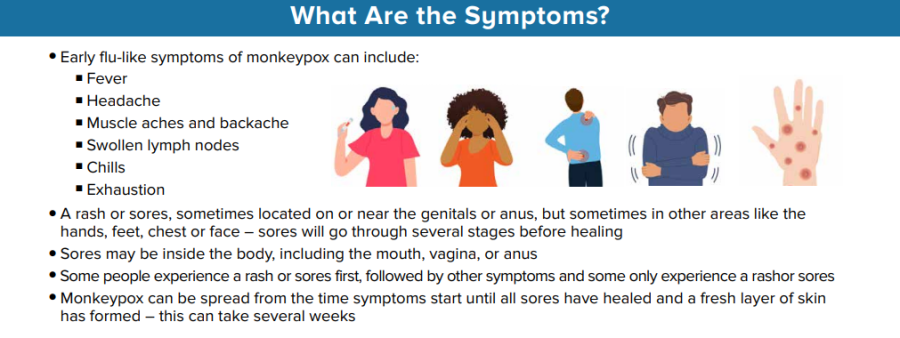
Symptoms usually last between 2-4 weeks and a health care official should be notified if the symptoms don’t improve or worsen. If someone thinks they may have monkeypox, they should notify a health care provider to help prevent further transmission.
How has the COVID-19 pandemic helped researchers keep track of and manage future outbreaks?
Because of COVID-19, the world still has active channels of communication with health departments, hospitals, surveillance laboratories, health care workers, researchers, policymakers and more, she explained.
“This has allowed for more direct education and awareness messages to be delivered to stakeholders so that everyone is aware of the outbreak, the signs and symptoms associated with infection, proper steps to record and report cases, and up-to-date research findings to fine-tune our approach.”
So, what now?
The CDC is tracking cases that have been reported in countries that don’t usually have monkeypox cases. Their data suggest that gay, bisexual, and other men who have sex with men make up a large population of the monkeypox cases.
“However, anyone who has been in close contact with someone who has monkeypox is at risk,” says the CDC in a 2022 overview.
The CDC is working with health officials nationwide to help identify those who may have had contact with those who tested positive for monkeypox and urge them to keep an eye out for patients with rash symptoms.
“We […] have a very public health-savvy population, both nationally and globally, who understand the epidemiological terminology associated with case investigations and outbreak response,” Dr. Barnes concluded. “This is incredibly helpful for public health organizations to share information and to ask for help in the identification and reporting of new cases and in our efforts to prevent new exposures and control the current outbreak.”
___
For more information or news tips, or if you see an error in this story or have any compliments or concerns, contact editor@unfspinnaker.com.