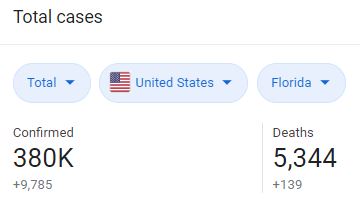
In the past few months coronavirus cases have surged in Florida, with over 380, 000 confirmed COVID cases as of today.
Many are rushing to the testing centers to know whether or not they have the virus, but will the results they receive be correct?
John Hopkins researchers calculated daily false-negative rates. They found that if a patient is tested too early, the results could come back as a false-negative: “Those tested with SARS-CoV-2 in the four days after infection were 67% more likely to test negative, even if they had the virus. When the average patient began displaying symptoms of the virus, the false-negative rate was 38%.”
The tests performed best eight days after COVID infection, but still had a false negative rate of 20%, meaning one in five people who contracted the virus was given a negative test result, according to the study. This would mean many who were tested in the early stage of their COVID infection would be told they were negative for the virus, but would actually unknowingly have the virus.
To understand how coronavirus testing works, we have to know what exactly is being tested in the first place. Spinnaker reached out to Kerry L. Clark, an Epidemiology & Environmental Health Professor from the Department of Public Health about the process of testing coronavirus:
“There are probably dozens of different versions of the SARS-CoV2 virus (COVID19) tests being used by different labs. When it comes to any clinical diagnostic testing, there are numerous details that can impact the validity of the testing. Two important characteristics are sensitivity and specificity of the tests. Two other important measures are positive and negative predictive value of the tests when they are applied to testing a specific population. There are epidemiological measures that are also somewhat technical,” said Dr. Clark.
Many coronavirus tests, called PCR testing, rely on the genetic material of the virus.
“I’m assuming that most of the COVID testing will be done to detect the genetic material of the virus, thus directly detecting the genetic footprint of the virus,” explained Dr. Clark. “This is the next best thing to actually culturing live virus in terms of evidence of an active infection.”
“False positives and negatives are possible with any type of clinical testing. There are a lot of coronaviruses in nature, so the tests have to be demonstrated as very specific for only SARS-CoV2. My opinion at this point is that false positives are probably not resulting too much from nonspecific amplification of other coronaviruses that patients might be infected with. False positives from DNA artifact contamination in the respective laboratories that are running so many of these tests every day is a reasonable concern, but that is always the case with PCR testing, and has to be managed by each lab’s protocols and workflow.”
Testing gone wrong could also relate to how virus samples are being contained and stored.
“Despite the incredible sensitivity potential for PCR testing, there are numerous ways to fail to obtain a positive result from a patient that is truly infected. There could be very low concentration of the virus (thus virus RNA) in the specific specimen obtained at the point in time of the sample collection. The specimen might not be handled properly, such that the viral RNA degrades prior to running the test. I worry about the long turnaround time for test results from some labs. Could the specimens be degrading during the long storage time? How are the samples stored during the wait time? I don’t know that any studies have been conducted to answer this question.”
Dr. Clark guesses that most of the COVID testing will be done with nasopharyngeal, or oropharyngeal swabs, or perhaps saliva – they will be a version of nucleic acid detection, not antibody tests. She also mentioned that some labs test fecal samples and have demonstrated, experimentally at least, that the virus can be detected in that type of specimen.
“But, I don’t know if that is being done routinely for clinical testing right now,” said Dr. Clark.
Dr. Clark says that only time and a lot of research is going to provide more accurate answers and clarification for these things. She believes that the safest approach is to assume that the test positivity rates are minimum infection level estimates, as most people being tested are symptomatic.
“The more severe the symptoms, the more likely someone will seek evaluation and be tested. This is the iceberg concept of infectious diseases, especially ones with highly variable presentation and a lot of mild or asymptomatic cases: as the bulk of the iceberg is below the water’s surface, so is the majority of the disease present in a given population,”explained Dr. Clark.
Hopefully, with time, all our coronavirus questions will be answered, but until then many of us can’t help but wonder: Does Florida really have 380,000 COVID-19 cases? Could we have less, or could we have a lot more?
If you’ve tested negative for a test, and are asymptomatic, it may be a good idea to wait at least a week to see if symptoms show, then get tested again.
There are many false positives and negatives in coronavirus testing, so it may be best to stay as cautious as possible. Practicing social distancing, consistently washing your hands, and wearing masks are all simple ways the public can contribute to limiting the spread of the virus.
__
For more information or news tips, or if you see an error in this story or have any compliments or concerns, contact editor@unfspinnaker.com.